ArthroRift: a day in the life of the wrist (volumetric rendering in VR for medical application). Medical students experience the complexity of the human body every day. They acquire a lot of physiological and anatomical knowledge in the course of their undergraduate studies. Part of this is the cutting room practicals where hands-on experience with anatomical structures is gained. Human anatomy is multifaceted and complex. This is particularly true for joints of the human body such as the ankle and wrist.
The starting point of this Grassroots application was the use of Virtual Reality (VR) as part of cutting room teaching with the aim of providing students with a better (spatial) picture in the structure and function of the wrist joint part of the first block in the third bachelor year “Diseases of the musculoskeletal system” and possibly in subsequent teaching.
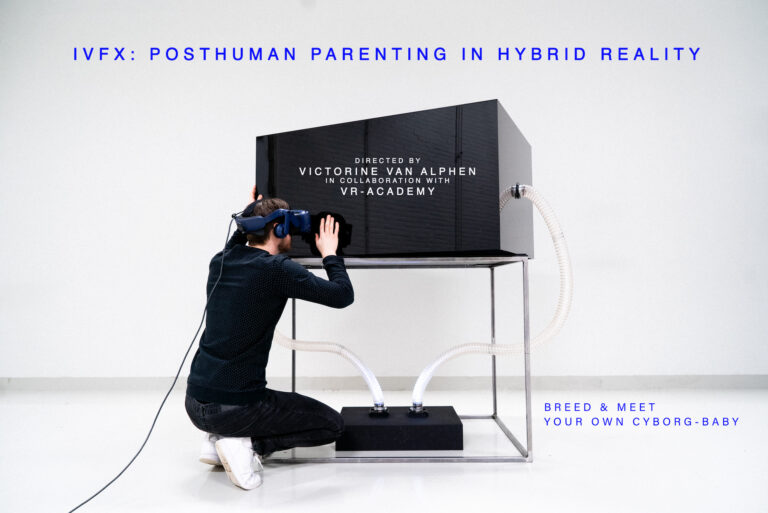
The first phase of the project, which started in January 2014, involved further exploration of VR technology and in particular the Oculus Rift. VR is a technology that allows the user to step into an alternate (virtual) reality. This often involves the use of special VR glasses, a ‘head mounted display’, which immerse the user in the virtual world. The Oculus Rift (http://www.oculusvr.com/) is an example of such glasses. You put on the glasses and stand in the middle of the wrist, so to speak.
A second phase of the project involved formulating and specifying the learning objectives of the application in consultation with the teachers involved in combination with the possibilities of the technology. This resulted in two educational settings for which the application can be used: during lectures of the “musculoskeletal disorders” block and in the continuing education of assistant physicians in the field of hand and wrist surgery. We explain the second context in more detail here.
A hand-wrist surgeon frequently uses arthroscopy of the wrist. In this operation, a small camera (an arthroscope) is inserted into the wrist that allows diagnoses to be made and a number of minor surgical procedures to be performed. To master this technique, trainee doctors first go through an e-learning module that explains specific knowledge about the procedure. He is then enabled to practice with a physical model of the wrist to train the appropriate skills. The following learning objectives have been established for the VR application:
- After attending the VR module, the trainee will be able to point out the important anatomical structures* from the radio-carpal space of a healthy wrist joint in the VR application image and in authentic arthroscopic image.
- After attending the VR module, the trainee will be able to navigate from the 3-4 portal to the important anatomical structures* in the radio-carpal space in the VR application by devising a safe and efficient pathway on their own based on anatomical knowledge of the wrist joint.
- After completing the VR module, the trainee will be able to perform a diagnostic scopy in the VR application where all relevant anatomical structures* are viewed from the radio-carpal space by following the taught route from the 3-4 portal.
In the third phase, we started developing the application. First, we created a 3D model of the wrist joint, ulna and radius. For this, we used a CT scan (of a physical remains of an adult woman). We then wrote an application in which the end user can use the Oculus Rift to view these anatomical structures. Finally, we simulated the control of the arthroscope using the computer mouse as a substitute for the inserted camera.
We also created an interface for the user that allows several options to be switched on and off. This allows different facets of the professional situation to be simulated to a greater or lesser extent. For example, the user can choose between moving freely or moving with the scope’s contraints. There are even more settings that increase and decrease complexity. Here, the content choice is between exploration of the wrist joint or simulation of an arthroscopy.
Description of how the application works
When starting the application, the user stands in the wrist joint. He can move by means of the mouse. In doing so, he is bound by the movement restrictions that the arthroscope has in real life as well. In addition, the user can use head movements to determine the orientation of his field of vision. This allows him to ‘look around’ as if he were really standing in the wrist.
Deployment of the VR application in medical education
The developed application will be used in medical education in three ways. A first used involves deployment during lectures of block 3.1. Here, the lecturer can show the VR application on a large screen to the student without using the Oculus Rift.
A second application concerns the use of the VR application as a practice station during cutting room practicals. This means that students can take turns using this technology to delve further into the anatomy and functionality of the wrist joint. For example, a student assistant might ask a student wearing the Oculus Rift: “follow the diagnostic pathway as performed during an arthroscopy of the wrist”. While this is expert knowledge, the excellent and/or interested student could go a step beyond the recommended study material here.
A third application of the VR application concerns its use for doctors in training to become surgeons. After gaining theoretical knowledge in an e-learning module, trainees can apply it practically in the VR application. In doing so, they can learn to link their anatomical knowledge to arthroscopic images. In addition, they can experience the movement limitations of the arthroscope and learn to deal with them. After practising with the VR application, trainees get to work on a physical simulator with real surgical instruments.
Team
The application was developed by Roland van Mossel (medical student) guided by a multidisciplinary team: Prof. Dr Mario Maas – Radiologist; Drs Roeland Kleipool – Associate Professor of Anatomy & Embryology; Dr Noor Christoph – Associate Professor of Educational Technology; Dr Geert Streekstra – Biomedical Engineer; Dr Iwan Dobbe – Biomedical Engineer; Dr Miryam Obdeijn – Plastic Surgeon. In addition, the National Aerospace Laboratory contributed to this project, for which thanks are due.